COVID-19 is here to stay. What can we do about it?
It’s become increasingly likely over the last several months, with the world grinding to a halt from this pandemic, that COVID-19 will not go away in 2020. The reality we live in now is that the SARS-COV-2 virus, which causes the disease, is probably too widespread and too infectious to simply disappear with the arrival of summer, and the earliest vaccines are at least a year away from mass distribution . History books will remember that we started the decade off with social distancing, hand sanitizers, face masks and toilet paper shortages, and that one little contagious bundle of RNA precipitated some of the widest acute behavioral changes we saw this century.
And yet, even amidst the extensive coronavirus lockdowns and with global authorities fully occupied provisioning medical supplies to treat infections, the world is finding its own ways to stay working and productive in this challenging time. Pathology is no different, having responded with immediate measures to keep pathologists and laboratory personnel safe while continuing to provide essential services to their communities.
Now, four weeks into widespread lockdowns in the U.S. and with a little more perspective, we must consider what it means to live with COVID-19 long term. Pathology carries many transmission risks in its daily workflow, even leaving aside medical conferences and international projects (which are no doubt mostly cancelled or put on hold). Whether it is traveling between client laboratories as a consultant, making the weekly rotation to satellite hospitals in the network, or even just going between the office and the bronchoscopy suite for adequacy checks – doing so while the patient is in the room for resampling – many regular routines of the pathology department put the pathologists squarely at risk of infection, and to be a potential vector of unwitting COVID-19 transmission.
That is why most pathology departments right now are scaled back on elective or non-essential procedures. However, this is arguably untenable in the long term as many of these procedures are lifesaving and can drastically alter patient outcomes. We should not have to choose between protecting pathologists and helping patients. Thankfully, this is where digital tools can help!
Many Digital Pathology companies today offer a wide selection of tools that enable remote slide sharing or image streaming. However, considering that the digitization timelines for many hospitals have been significantly accelerated by COVID-19, some organizations may be only now considering digital tools seriously for the first time. The choices can be overwhelming, and so we have put together a summary of the main types of digital tools to help you navigate the available options.
Scanned Digital Slides – Seemingly the most obvious answer to the phrase “digital workflow”, digital slides can be scanned and digitally shared for second opinions, education and training, and, in cases where the system is FDA approved, can be used for sign-outs.
- Pros: FDA approved scanning systems are available today with various vendors*
- Cons: Can be incredibly expensive to test or adopt. High volume scanners cost hundreds of thousands of dollars each, and require substantial additional IT investment to onboard. Scan times and focus issues may make this option not suitable for rapid evaluation samples or cytology sharing.
Cloud Consultation Platforms – International collaborations can leverage cloud technology to bridge the physical distance between sites to continue their work, whether it is humanitarian or otherwise. The ASCP Partners in Cancer Diagnosis program is one notable success case.
- Pros: Can eliminate the need for international travel.
- Cons: Bandwidth issues and hosting can be challenges. Scanner reliability is key for remote deployments. Cloud platform costs can vary significantly.
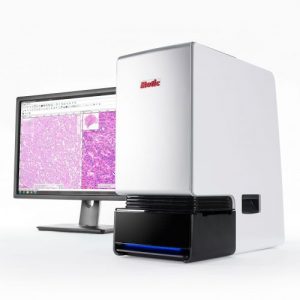
Live Image Scanners – Some scanning systems can also be turned into robotic microscopes which can be streamed and controlled remotely, in real time, eliminating the need to wait for a scan to complete. These systems allow the pathologist to retain full x, y and focus control over the sample, and can be particularly useful for rapid evaluations or in cases where the sample is thick or uneven.
- Pros: Pathologist retains live control of the sample. Least complicated to implement, and typically much less expensive since the systems are low volume or single slide capacity.
- Cons: Designing good controls can be tricky due to over-the-internet lag. Frequent focus adjusting may be required in systems without adaptive autofocus.
Video Microscopy – The simplest digital tool: mount a camera on a microscope and stream the image to the pathologist via video chat. A technician is required onsite to control the microscope for the pathologist.
- Pros: Generally the least expensive method.
- Cons: The pathologist has no control. Requires intensive training to work; operating the microscope for a live stream audience is very different from using one normally in clinical practice. Fewer digital features, no option for scanning.
Imagine having to do this without the Internet…
Motic is committed to supporting the medical community through COVID-19 by empowering hospitals with digital tools to reduce unnecessary travel and risks while maintaining the same standard of care for patients. Interested in learning more about Motic’s telepathology platform? Contact us for a demonstration, or click here for more information about our FS-Live system.
*Motic scanners are not FDA approved for primary diagnosis