While the term digital pathology has been around for nearly two decades, we are only just starting to see widespread acceptance of this healthcare technology concept. For long-time advocates who’ve been mapping the Gartner hype cycle for digital pathology, it may feel as though the idea never even experienced a peak “inflated expectations” phase before falling into the “trough of disillusionment.”
When we look at the history of digital pathology, we see that, for years, the list of reasons not to adopt telepathology far outweighed any perceived return on investment. And it didn’t help that some early adopters felt burned by the cost of digital pathology scanners and microscopes with unclear pathology applications and limited value-add. Healthcare as a whole grew understandably wary of companies promising the next big disruption in pathology when the results seemed both distant and unproven.
Today, however, pathologists are beginning to embrace the prospect of going digital more than ever before.
So, what’s changed?
For one, technology is finally catching up to the promises of digital pathology solutions. Faster scan times, sharper optics, and more reliable internet connections have all contributed to creating scanned whole slide images with a level of accuracy that pathologists feel comfortable using for research and consultation.
Secondly, and unfortunately, the global pathologist gap is rapidly increasing, with developing countries hit hardest. The World Health Organization notes that in 2017 only 26% of low-income countries reported having pathology services generally available in the public sector. And even wealthy areas are experiencing large pathology provider shortages, with most health organizations projecting no turnaround in the coming decades.
In the face of these shortages, pathologists moved from thinking of digital medicine as an interesting but distant theoretical toward understanding it as a transformation that offers pressingly urgent interventions for the here and now. Clinicians who connected with distant colleagues for teleconsultation, researchers who incorporated high-volume WSI scanners into their work, and pathology departments that trained medical students using digital slide imaging have all been key to lowering the acceptance threshold for everyone else.
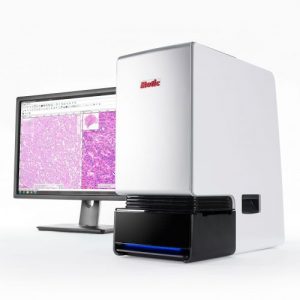
Finally, as our retrospective of USCAP 2019 pointed out, a key component to changing perceptions has been showing pathologists how the innovations that are driving digital pathology’s future can nevertheless be used in practical ways in the present. We’ve all heard horror stories of digital pathology early adopters who bought a scanner but then ended up with, effectively, a very expensive doorstop or bookend because they weren’t offered practical, easy ways to implement these digital pathology devices into their daily workflow.
There are many exciting developments for telemedicine right on the horizon, especially with the turn towards pathology diagnostic machine learning. But no industry can move faster than its end users. The course correction toward targeted, specific applications that pathologists can use today was a necessary development to create the levels of trust and buy-in that we are now seeing.
With pathologists increasingly accepting that a turn to digitization is both inevitable and valuable, the pathology industry must now address the hows of digital pathology implementation. In upcoming posts, Motic will offer more insights into the practical steps towards widespread digital pathology use. Subscribe to Motic’s newsletter below to learn more.